Drug development is a complex process of exploration that calls on researchers to work together to blaze new trails in science. Using cutting-edge technologies and methods, drug discovery can lead to major breakthroughs against diseases that afflict millions of families, from Alzheimer’s to cancer.
Right now, the field is focused on addressing the COVID-19 coronavirus pandemic that has upturned families, businesses, communities, and the global economy. More than 500 clinical trials are underway across the globe to test vaccines and treatments, enrolling thousands of participants.
However, modern healthcare has long been plagued by problems of access, equity, and even outright discrimination. Take the Tuskegee experiment as an example. These issues continue to haunt the research enterprise and have contributed to a lack of diversity in research studies for new drugs and treatments.
This is problematic on many levels. In the case of COVID-19, it is clear that the virus disproportionately impacts black and Latino families. In fact, Latinos in New York – the epicenter of the crisis – are dying at the highest rate.
This data raises key questions related to health equity in testing, treatment, and research. Why are tests not reaching these communities? Will these communities equally benefit from emerging efforts to digitize contract tracing? Are these communities adequately represented in the COVID-19 trials underway in the U.S.?
As the research field grapples with these questions, it is possible to look to other disease areas such as Alzheimer’s for guidance on how to avoid missteps.
Latinos and African Americans make up less than 20 percent of participants in federally funded Alzheimer’s research, despite being 1.5 and 3 times more likely, respectively, to develop the disease compared to non-Hispanic whites.

Diversity in clinical research is critical to developing effective treatments. Racial and ethnic differences can relate to disease pathology and impact the effectiveness of drugs. For example, up to 75% of Pacific Islanders are unable to convert the blood-thinning drug clopidogrel into its active form and are at higher risk for adverse outcomes. Will this be the case with a COVID-19 vaccine and new treatments?
Despite its importance, the lack of representation of racial and ethnic minorities in research has long been overlooked by industry, policymakers, and even the public. It wasn’t until 2012 that Congress required the U.S. Food and Drug Administration (FDA) to report on the diversity of participants in clinical trials and the extent to which safety and effectiveness data is based on demographic factors such as sex, age, and race.
Low levels of representation underscore the need for structural changes in how industry – and government – engage diverse communities. We recently wrote in STAT News about ways the Alzheimer’s field can prioritize inclusion and we have now revised these lessons to help guide an equitable response to our nation’s COVID-19 response.
- Collect and release subgroup data. Despite a higher risk for COVID-19, African Americans and Latinos have limited access to testing. Congress should direct the Department of Health and Human Services to collect comprehensive, demographic data on race/ethnicity and language of patients being tested, the rate of positive test results, and outcomes for those with COVID-19. This data will be invaluable to ensuring that our nation’s health response to the current crisis is equitable and reaching all communities.
- Expand paid leave benefits in any future COVID-19 response legislation to support the millions of family caregivers impacted by the coronavirus. A new UsA2 flash poll on how the Alzheimer’s community has been impacted by COVID-19 finds that 70% are concerned about their finances and their family’s finances during this crisis. These communities have largely been left out of the Families First and CARES Acts. Read our letter to Congress on this issue here.
- Broaden the criteria for research eligibility and allow for flexible study protocols to address barriers that often stand in the way of Latinos and African Americans qualifying for research. Strict eligibility criteria for trials can lead to limited representation of minorities in clinical research, especially given the multiple chronic conditions that African Americans and Latinos often face. The FDA has issued guidance on modifying study protocols in light of COVID-19.
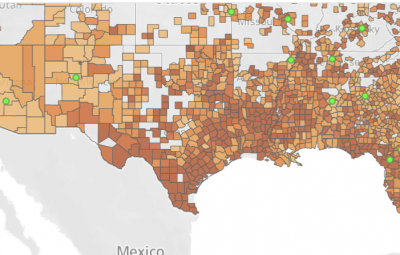
- More effectively leverage data on the social determinants of health and research infrastructure to identify and engage higher risk communities. Collecting and mapping data on social determinants of health in relation to disease impact can help the field better understand and address gaps in research and health services.
Without addressing the equity and access gaps that persist in our drug development process, our nation will never make equitable progress against health threats like COVID-19 and Alzheimer’s. Without change, our nation’s inaccessible research enterprise will call into question our true commitment to science and better health for all.
Stephanie Monroe is executive director of AfricanAmeriansAgainstAlzheimer’s and a former Department of Education Assistant Secretary for Civil Rights and Jason Resendez is executive director of LatinosAgainstAlzheimer’s networks of UsAgainstAlzheimer’s.